Abstract

Introduction: Autoimmune hemolytic anemia (AIHA) is a rare condition that can cause potentially serious complications in pregnant women and newborns. With the lack of prospective trials, physicians often have to make treatment decisions for this vulnerable population based on scarce literature with poor evidence. We sought to summarize existing literature and analyze maternal and neonatal outcomes in pregnancy-associated AIHA (p-AIHA).
Methods: Cases of AIHA in pregnancy were collected using MEDLINE/PubMed and Google Scholar literature search using terms "autoimmune hemolytic anemia" and "pregnancy". Bibliography of each article was hand-searched for additional reports. Only publications in English were included. Cases of preexisting AIHA, autoimmune disease associated AIHA, non-immune hemolysis, and cases where direct antiglobulin testing (DAT) was not performed, were excluded. Laboratory, obstetric, neonatal and treatment data were collected. Data were analyzed using descriptive statistics. We used Wilcoxon rank sum test for continuous variables and Fisher's exact test for categorical variables. When missing data were encountered, we reported a valid number of analyzed patients in parentheses.
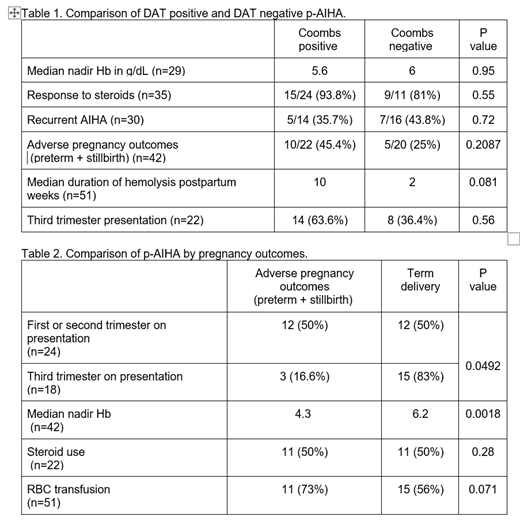
Results: We identified 87 cases of p-AIHA from case reports, case series, abstracts and posters. Final analysis included 51 individual women. Median age at p-AIHA presentation was 28 years. Presentation was less common in the first pregnancy (34%); most cases presented in the second or third trimester (83.3%).Median nadir hemoglobin (Hb), lactate dehydrogenase, total bilirubin and peak reticulocyte count were 5.8 g/dL, 457 U/L, 2.2, and 13.6%, respectively. DAT negative hemolysis was reported in 41% of cases (Table 1). DAT positivity was not associated with pregnancy trimester, hemolysis severity, response to steroids, AIHA recurrence, adverse pregnancy outcomes, or hemolysis in newborn. There was a trend for longer duration of hemolysis postpartum in women with positive DAT compared to negative DAT (10 vs 2 weeks, p = 0.08). Median duration of hemolysis postpartum was 6 weeks (n=27, range 0-96 weeks). Two thirds of women were treated with steroids with hemoglobin response of 88.9% (n=27). There was no association between steroid use and duration of hemolysis postpartum. Blood transfusion was administered in 27 out of 33 women, with a median number of units transfused 5. Recurrent p-AIHA was seen in 40% (12/30) of women; there was no difference in nadir Hb levels for those with recurrent p-AIHA vs. not recurrent (6.8 vs 5.2 g/dL, p=0.11).
Pregnancy resulted in term delivery in 61.9%, preterm delivery in 23.8%, and stillbirth in 9.5% (n=42). Adverse pregnancy outcomes, which included preterm labor and stillbirth, were reported in 50% of women who presented in the first or second trimester compared to 16% who presented in the third trimester (p=0.049, Table 2).Women with adverse pregnancy outcomes had significantly lower median nadir hemoglobin compared to women without adverse pregnancy outcomes (4.3 and 6.2 p = 0.0078) and were more likely to receive transfusion (73% and 56%, p= 0.071). Hemolysis at birth was reported in 59% (n=22) of newborns with available data with 13 neonates (38%) requiring transfusion support . Use of steroids had no effect on presence of hemolysis in the newborn.
Conclusions: We present the largest cohort of p-AIHA described in the literature. Our study reports that p-AIHA is uncommon in primigravidas and typically presents later in pregnancy. Presentation in first or second trimester in pregnancy and lower Hb nadir were significantly associated with adverse pregnancy outcomes. Steroids and blood transfusions were needed in most patients, and hemolysis persisted on average for 6 weeks postpartum. There was a high frequency of Coombs negativity which was associated with shorter duration of postpartum hemolysis. Preterm labor and stillbirth were observed in 33.3% of pregnancies. The incidence of hemolysis in newborns from p-AIHA mothers is very high and is often clinically significant. Recurrence in subsequent pregnancy is common but has similar Hb nadir as non-recurrent cases. This study provides insights into the clinical course of pregnancy and neonatal outcomes in p-AIHA. Our findings may help guide management of this rare condition. A prospective study of patients with p-AIHA is needed to determine optimal therapy to reduce antepartum and neonatal complications.
Murakhovskaya: Alexion, Rigel, Bioverativ/Sanofi, Momenta, Annexion, Incyte: Research Funding; Bioverativ/Sanofi, Momenta, Apellis, Novartis: Consultancy; Cardiff Oncology, Trillium Therapeutics: Current holder of individual stocks in a privately-held company.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal